|
Getting your Trinity Audio player ready...
|
In light of dwindling rural healthcare access, an Auburn University program is seeking to use emerging technologies to fill gaps in the state’s rural healthcare systems.
The Auburn University Rural Healthcare Initiative is a program started by the university in 2020 to address health disparities faced by rural Alabamians.
Dr. Hollie Cost, program director and assistant vice president for Auburn University Outreach and Public Services, told APR the program has used telehealth technologies and local community leadership to fill coverage gaps that leave many rural Alabamians without easy access to medical services.
The initiative currently offers healthcare services across 13 counties. This includes free access to OnMed Care Station telehealth booths at five locations in Gainesville, Boligee, Shaw, Akron and Lafayette.
OnMed Care Stations give patients access to a private booth connected via video chat to a real physician and medical devices which capture a patient’s vitals to aid them in diagnosis.
“It’s just like a phone booth, and it has a walk-in, and you get complete privacy because the windows can fog over,” Cost said, describing the telehealth stations. “You have this life-size person so you can really make connection with them.”
Cost explained that, during her time at the initiative, she encountered many Alabamians unfamiliar of the extent to which healthcare access is a struggle for rural citizens.
“People don’t understand that not everyone has this easy access to healthcare. Even if it’s right down the road they may not have insurance,” Cost said. “They may not have transportation, and it seems to me like it’s really challenging for some people to look through the lens of others if they’ve never walked in their footsteps or if they’ve never been in these communities and really seen just how rural they are.”
Cost’s assistant and AU Health Initiative worker, Kate Bouchillon, explained healthcare access is particularly difficult for Black Alabamians living in rural communities.
“There is a disparity of resources being allocated to these communities that are more populated by African Americans,” Bouchillon said.
Bouchillon explained that alongside a lack of healthcare access, generational distrust of medical professionals as a result of the historic mistreatments, such as The Tuskegee Syphilis Experiment, have made health outcomes consistently worse in Alabama’s predominately Black rural communities.
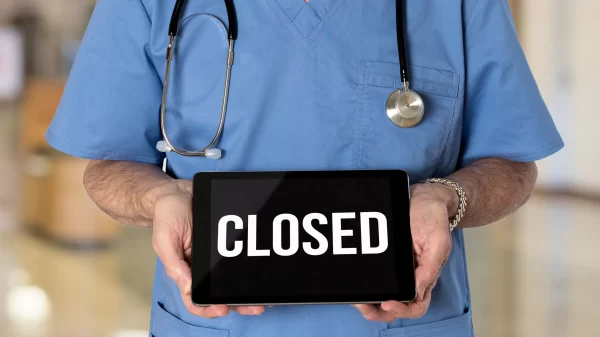
A University of Alabama study found that, of the 24 counties in Alabama’s Black Belt, 17 were below the statewide average of 3.9 hospital beds per 1,000 residents, with four of these counties—Lamar, Lowndes, Perry and Pickens—having no hospital at all.
According to the Alabama Hospital Association, seven rural hospitals have closed in the state since 2011.
A report from the Center for Healthcare Quality and Payment Reform found over half of the state’s 52 rural hospitals to be at risk of closing, with 19 at an “immediate risk.”
In recent months, Lawrence Medical Center in Lawrence County ended emergency room and inpatient services, while Thomasville Regional Medical Center in Clarke County suspended all operations due to staff shortages.
Recent cuts and layoffs faced by the National Institutes of Health and Centers for Disease Control at the request of the Trump administration’s Department of Government Efficiency have raised concerns amongst Alabama healthcare providers regarding the future of rural healthcare.
A proposed 15 percent cap on indirect cost payments made to help hospitals and research institutes pay their administrative costs would take millions of dollars in funding from the University of Alabama in Birmingham’s health systems and healthcare institutes across the state.
NIH is the largest funder of federal medical research in the U.S. The institute sent UAB alone $407 million in 2024. Health institutions across Alabama received a total $909 million in funding from NIH in 2023. UAB’s current overall indirect cost rate provided NIH is 33 percent.
A preliminary injunction filed by a U.S. District Court judge has blocked the new indirect cost rate’s enactment.
Officials from UAB, however, have alleged that the proposed cuts to NIH funding would cost UAB $70 million a year and put jobs and lifesaving research provided by the university at risk.
Recent cuts to the U.S. Department of Health and Human Services have also slashed $239 million in Alabama public health and research grants.
Cost said that although the rural healthcare project was not affected by recent federal cuts requested by DOGE, she feels they may very likely negatively impact healthcare coverage across the state.
“I think it could potentially be devastating just because, yeah, the funding, the systems and mechanisms are already so unstable, and in a state that hasn’t expanded Medicaid and we’re really hurt, so it could be devastating,” Cost said. “Luckily, we have kind of this multi-prong funding source where we have some university funding, we have some from the state and then we have some federal trickle down through some grants that we’ve secured.”
According to Cost, however, some of the program’s 2025 funding has been put on hold due to the U.S. Congress’s continued debate over the federal budget for 2025.
“There’s one particular funding source that, because of the congressional continued resolution for the budget, there’s some funding that we were counting on that will not be allocated to us right now,” Cost said.
Cost explained the initiative is looking at more private funding sources after losing some federal funding, but expressed concerns that private funders will be unable to fill the gaps left by sweeping federal cuts.
“They’re gonna be tapped from all different directions, and so some folks that we may be able to depend on in the past, you know, I get concerned that they’re being stretched too thin,” Cost said.
Cost also said while federal grants have been inefficient in addressing the state’s healthcare issues, she believes widely slashing federal funds will only worsen healthcare disparities.
“The old way wasn’t working, I mean, but I don’t think you throw the baby out in the bathwater, and I don’t think you do it the way that it’s being done,” Cost said.
Discussing the future of Auburn’s rural healthcare services, Cost said the initiative has been working with community leaders to help support those without the access to transportation necessary to receive medical care.
“We have a good network of the Chambers County, that they might give their friends rides which is nice,” Cost said. “And then also churches—we’re getting churches involved.”
According to Cost, religious leaders have helped improve transportation access and through the Rural Healthcare Initiative’s Health Temple Initiative, which encourages faith leaders to emphasize the importance of healthcare to their congregations.
The initiative also continues to look at new technological innovations to make their coverage more robust.
Cost explained that this includes a recent grant that has allowed the initiative to purchase Medpod Health telehealth carts, which can be transported into patients’ homes.
She also said the initiative has been exploring further ways they could potentially improve rural patients’ transportation access.
“Right now, it’s really just a dream, and there are some options out there for potentially creating an Uber-like app in rural areas but there’s just so many hurdles to jump through with that,” Cost said.
Cost said the initiative has also looked at expanding services offered in OnMed stations by adding mental health care services and an otoscope for ear screenings.