After the Alabama Supreme Court ruled that frozen embryos used for in vitro fertilization (IVF) treatment were to be considered human beings in February of this year, the future of IVF access in the United States has been thrown into question, with both political parties fighting to position themselves as the true supporters of IVF.
Earlier this month, the Fertility Providers Alliance (FPA) — an organization established by providers of reproductive medicine to “expand access to care, deliver high quality fertility services, and continuously advocate for our patients” — held a virtual press conference to discuss the future of IVF treatment ahead of President-elect Donald Trump’s return to the Oval Office.
The conference began with Matthew Maruca, the Chief Legal Counsel at Inception Fertility and an FPA contributor, describing the fallout of the Alabama Supreme Court ruling.
“That set off a bit of a political firestorm that thrust IVF into the public policy spotlight and into the political discourse throughout the election season,” Maruca said. “We noticed that, in monitoring these developments, that there had been numerous proposals that could impact IVF. Things such as limiting the number of embryos that could be created, limitations on the types of genetic testing that might be available, or restrictions on the ability to discard or transport tissue or cryostore tissue.”
“We felt, as a group, that these public policy discussions often lacked an understanding of IVF and its limitations and its capabilities or were otherwise incomplete,” Maruca continued. “These have resulted in proposed legislation that could be restrictive to family building and have caused a great deal of patient anxiety and concern.”
Maruca specifically highlighted lower IVF success rates, fewer children, and higher patient costs as negative downstream effects that could be wrought by legislation proposed in states like Texas, Louisiana, and Alabama.
Paul Dudley, a provider at Pinnacle Fertility in Atlanta, and Christine Mansfield, the medical director at Aspire Fertility in Dallas, went on to provide an in-depth look into the IVF process and debunked myths and misconceptions about the treatment.
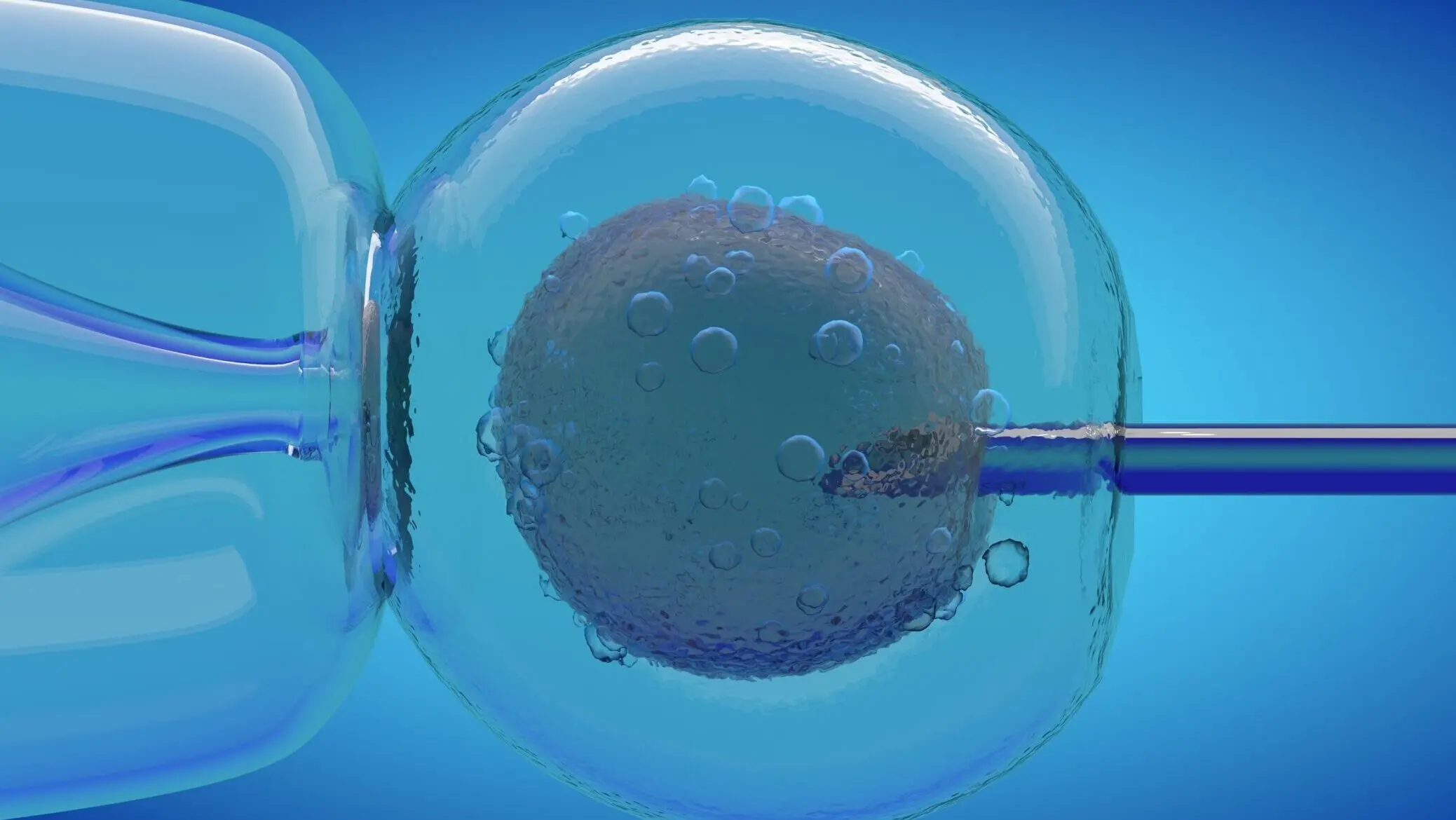
Dudley explained that infertility is a disease affecting millions of Americans and that IVF is a means of treating that disease. He added that the eggs used in IVF treatment are ones which would have normally been reabsorbed by the body and that the genetic testing involved in modern IVF allows providers to reduce the occurrence of miscarriages and genetically abnormal pregnancies.
Mansfield elaborated on Dudley’s discussion, sharing how IVF providers are actually just “mimicking exactly what nature does” — the only difference being that the development of embryos can be observed under the microscope and that failed pregnancies can actually be better avoided.
“One of the things that seems to be a common misconception is how efficient human eggs are,” Mansfield said, emphasizing just how many embryos fail to attach to the uterus or go on to miscarry naturally. “[Producing a viable pregnancy] can take, easily, four natural cycles if everything’s perfect.”
For women who are older or obese, it can take even longer to produce an embryo that effectively implants into the uterus and goes on to be a viable pregnancy. While the body can only test one embryo at a time for viability, IVF can test a host of embryos all at once — reducing the time it will take to produce a successful pregnancy while dealing with the same odds of producing a viable embryo that the body would naturally. The embryos discarded in IVF are the same embryos that the body itself would naturally discard as nonviable pregnancies.
Mansfield explained that IVF treatment with preimplantation genetic testing (PGT-A) significantly reduces pregnancy loss and results in a higher birth rate. The rate of success with IVF that employs PGT-A has only grown as that technology has improved over time. 1.6 million children have been born in the United States through IVF with PGT-A since 1987.
Next to speak was Ineabelle Collazo, the lab director at IVFMD Florida, who dispelled the false narrative that IVF clinics are underregulated. Collazo explained that providers are subject to federal oversight by bodies like the CDC, FDA, and CMS, in addition to professional oversight from the College of American Pathologists, the Society for Assisted Reproductive Technology, and the Joint Commission on Accreditation of Healthcare Organizations.
Lastly, Tiffani White, a patient from Atlanta, GA, spoke to share how IVF helped her overcome infertility to become pregnant after 10 years of trying to start a family.
“I’m grateful, I’m overwhelmed with joy to have had access to such medical technology like IVF, to give someone like me a chance to have a biological child to carry and experience my dream of motherhood,” White said.
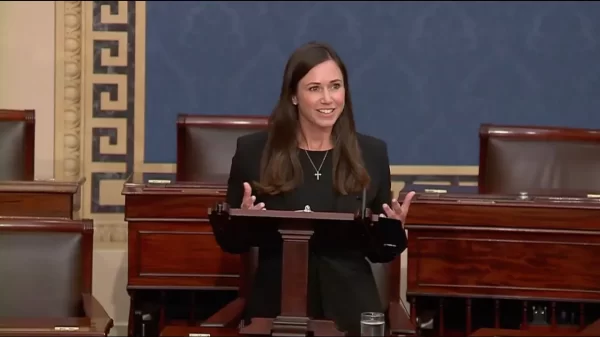
Although President-elect Trump has publicly stated that he will be a “LEADER on I.V.F.” and that his administration “will be great for women and their reproductive rights,” it remains unclear how those comments will translate into policy and whether his administration will actually work to protect IVF access. In September, Trump’s Republican allies in the U.S. Senate blocked a bill that would have codified IVF protections into law and mandated insurance coverage of related procedures.
Additionally, Trump is responsible for appointing three justices to the U.S. Supreme Court during his previous term in office — the same Court which blocked an IVF clinic’s appeal of the Alabama Supreme Court’s February ruling earlier this year and previously overturned Roe v. Wade in 2022.