For patients in Alabama and throughout the nation, the high costs of health care can often create needless emotional and financial stress. Surprise medical billing—in which patients receive outrageous bills in the mail weeks or months after inadvertently receiving out-of-network care—only adds insult to injury.
No one should have to worry about getting hit with high medical costs twice—which is why Congress has a duty to solve this issue. In doing so, they should take an approach that benefits the average American, not some huge insurance company. Unfortunately, some of the measurers Congress is considering take the opposite approach.
One terribly misguided proposed solution would tip the scales against local doctors and their patients and in favor of large insurers and the managed health care industry. This proposal—known as benchmarking—would essentially permit the government to set arbitrarily low out-of-network rates for physicians by basing them on insurers’ highly discounted in-network averages.
While on its surface this may appear to protect patients from out-of-network billing disputes, it would also create a massive imbalance in our health care system that would give insurers more leeway to slash reimbursements to, and sever contracts with, doctors. That would result in even smaller provider networks, meaning less access to in-network care for patients (in other words, even fewer healthcare options for patients)—the exact opposite of where we should be headed.
Not only that, but by drastically reducing rates for doctors, benchmarking would dump huge financial losses onto local health care facilities like ERs and hospitals. Many of these facilities are struggling as it is – especially in rural parts of the state and country. A benchmarking approach could worsen an already dire doctor shortage or lead to more hospitals closing their doors, once again reducing access for patients while driving costs even higher.
Vulnerable patients and their families deserve a better solution. Luckily, Congress is also considering other measures that include a far more even-handed, patient-centric approach. Called Independent Dispute Resolution, or IDR, this approach would allow both insurers and physicians to have a say in the process. In the case of disputed out-of-network services, IDR incentivizes both parties to submit their most reasonable payment amount through an open, transparent, and online process overseen by a neutral, unbiased mediator.
Within 30 days, this mediator would make a final decision regarding payment amounts based on each party’s offer and a range of factors that determine the true cost of care in a given location or facility type. As an extra bonus, interim, market-based payments to providers at the onset of the IDR process would help keep at-risk rural hospitals financially stable and secure, protecting access and affordability for communities that need it most.
Not only would IDR help determine fair rates that accurately reflect the cost of clinical services, it would provide additional incentives for insurers to negotiate fairly with physicians in order to grow their provider networks. This would help address one of the key issues that is driving the increase in surprise medical billing: network adequacy. Patients deserve to have robust provider networks that give them access to more in-network physicians, ER doctors, and specialists. IDR would help ensure they do.
For proof of IDR’s efficacy, all Congress needs to do is look to New York to see how well their IDR-based law, enacted in 2015, is working. Since the law’s passage, out-of-network rates have dropped by 34 percent, and in-network emergency care costs have dropped by 9 percent. It is ironic that the managed care industry as a whole would be calling for the flawed benchmarking solution when even the New York Health Plan Association has been a vocal advocate for IDR.
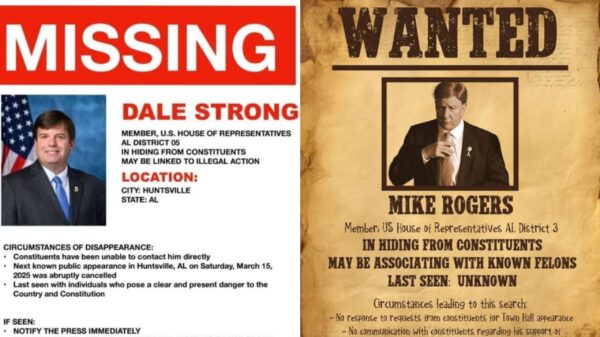
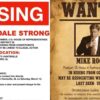
Rather than simply pushing through a flawed bill or attaching surprise billing to some unrelated legislation, Congress needs to take the side of the average American here and pass legislation that includes the IDR framework. I trust we can count on Representative Terri Sewell and our congressional delegation to help champion the IDR process and work with their colleagues to incorporate it into a comprehensive legislative solution that protects patients in Alabama and across this great nation.
Craig Ford is the owner of Hodges-Ford Insurance and the Gadsden Messenger. He represented Gadsden and Etowah County in the Alabama House of Representatives for 18 years.