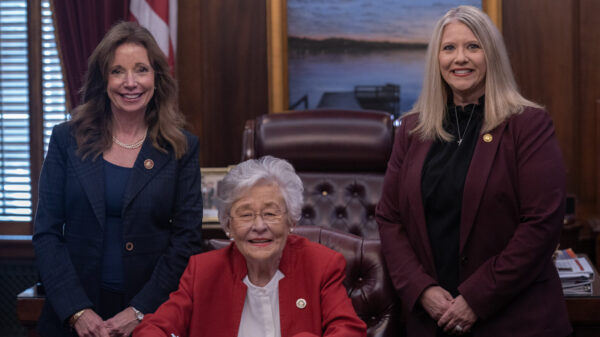
U.S. Rep. Terri Sewell, D-Selma, authored an article in “Modern Healthcare” on the growing doctor shortage and how it impacts Americans — particularly those living in rural areas.
“On top of rising medical and prescription drug costs, many Americans must travel long distances to access quality medical care because too often rural areas struggle to attract healthcare providers, especially those who are reflective of the communities they serve,” Sewell wrote. “Too many Alabamians—like residents of other parts of the country—cannot afford the cost and time it takes to visit the nearest provider, sometimes over an hour away.”
“Studies have long shown that the U.S. is not producing enough physicians to meet current and future needs,” Sewell added. “The Association of American Medical Colleges estimates that we will face a shortage of more than 121,300 primary-care and specialty physicians by 2030.”
To combat this growing problems Sewell introduced the Resident Physician Shortage Reduction Act of 2019, with Republican Rep. John Katko of New York. The bill would increase the number of Medicare-supported residency positions by 3,000 each year for the next five years, for a total of 15,000 new positions.
“This increase in residency spots would be an essential first step to ensure that every American, especially those in rural and underserved communities, has access to a well-trained physician,” Sewell wrote. “Our bill also requires the Government Accountability Office to study strategies to increase diversity within the health professional workforce. In minority communities, especially those in which men and women see themselves reflected in the long history of deliberately discriminatory and life-threatening practices, such as the Tuskegee experiment, mistrust of the medical community can cause families to stay home rather than seek regular care or participate in clinical trials and medical research that result in cures. As a result, curable diseases and illnesses go untreated and entire communities are left out of the greatest medical advances of our time.”
“Supporting a diverse pool of qualified physicians is a critical step in reviving trust lost by the ill effects of historical exploitation of minority communities in the medical field and eliminating racial disparities in health outcomes,” Sewell stated. “As many residents in rural areas are painfully aware, the number of doctors in our communities is not just a measure of privilege, it is a matter of life and death.”
The growing doctor shortage is recognized by both liberals and conservatives.
Dr. Kevin Pham, MD, is the summer 2018 Graduate Health Policy Fellow at The Heritage Foundation.
“Factors contributing to physician shortage include both recruiting new doctors and keeping current physicians interested in their practice,” Dr. Pham wrote. “Physicians, by and large, go into medical practice to enjoy the profound personal and professional satisfaction of serving a patient, and restoring a patient back to health. The essential health care interaction occurs between the physician and the patient, and anything that interferes with that relationship makes the best practice of medicine harder. The legitimate demands of patient care alone are a stressor endemic to the vocation, but adding the constant, intrusive interference of medical practice by third parties is corrosive, and can manifest itself in the job-killing phenomenon of “burnout.”
Dr. Pham wrote that a “Medscape survey also found that the largest proportion of physicians, 56 percent, felt that “too many bureaucratic tasks (e.g., charting, paperwork)” contributed to burnout; 39 percent pointed to being overworked; 26 percent pointed to lack of respect from administrators, employers, colleagues, or even staff; and 24 percent pointed to the increased computerization of medical practice in the form of EHRs.”
Pham cited a study that shows that rural areas, in which 19 percent of the U.S. population lives, have only 10 percent of the practicing physician population.
“Today, America is faced with the very real threat of a shortage of medical professionals to serve the needs of a growing and aging population of patients,” Pham warned. “America’s physicians are under stress, and many are demoralized, burned out, and looking toward an early retirement. Their problems have very little to do with actually delivering medical care to patients. They have much more to do with the non-clinical requirements imposed on them while running a medical practice. The survey data is quite clear: The laws, the rules, and the regulations that have interfered with the doctor–patient relationship have driven American physicians’ morale lower, and encourage them to leave medical practice at precisely the time the American people need them more and need them most. For policymakers in Washington and in the states, there is a serious lesson here: Any serious reform must shift the focus back to the patient–doctor relationship, unburden the practice of medicine, and let doctors be doctors.”
To read Sewell’s full column, click here.
Congresswoman Terri Sewell represents Alabama’s 7th Congressional District.